The fact is, 28,7% of seniors fall at least once a year ( 29.0 million falls ) from which 3 million are treated in emergency departements.
The incidence of falls among older adults is a significant public health concern.
Falls can lead to severe injuries, such as fractures and head trauma, decreased quality of life, and increased mortality.
Therefore, preventing falls is an urgent priority in senior healthcare. That’s why the risk of fall should be assessed.
A fall risk assessment is a systematic process by which healthcare professionals evaluate an individual’s risk of falling. This evaluation takes into account a variety of factors, including the person’s physical health, mental state, environment, and medications.
Based on this assessment, healthcare providers can implement interventions designed to reduce the senior’s risk of falling.
Through this article, we aim to dive deeper into the fall risk assessment process, who conducts these assessments, when it should be performed, and what factors are considered in the assessment and this through some of the most popular fall risk assessment tools.
Who Conducts Fall Risk Assessments
Fall risk assessments can be conducted either by a team of healthcare professionals who are responsible for a patient’s care, each bringing a unique set of skills and expertise to the process, or by a single professional.
The goal is to identify potential risks and develop strategies to minimize the chance of a fall. Here’s an overview of the key players involved:
Nurses: They often perform an initial evaluation when a patient is admitted to a healthcare facility, such as a hospital or nursing home.
Physical and Occupational Therapists: Therapists can evaluate a patient’s balance, strength, mobility, and ability to perform daily tasks.
Geriatricians: As physicians specializing in elderly care, geriatricians frequently assess fall risk, especially in outpatient settings or during routine health check-ups. They consider various factors, including chronic health conditions, cognitive function, and medication side effects, when assessing a patient’s risk.
The collaboration among healthcare professionals ensures a better approach to fall risk assessment. For example, nurse can get the help of pharmacists to review a patient’s medication regimen for any drugs that could increase the risk of falls due to side effects like drowsiness, dizziness, or disorientation.
When to Conduct a Fall Risk Assessment
The timing of these assessments is crucial and is typically dictated by specific events or conditions in a patient’s healthcare journey. Here are some of the critical times to perform a fall risk assessment:
Upon Admission to Healthcare Facilities
When a patient is admitted to a hospital, nursing home, rehabilitation center, or other healthcare facilities, this assessment forms a baseline for understanding the patient’s risk factors for falling and allows for the immediate implementation of any necessary fall prevention strategies.
It is also a fundamental part of care planning and informs healthcare professionals about potential challenges they might face during the patient’s stay.
After a Significant Change in Health Status
Significant changes in a patient’s health status, such as after surgery or a severe illness necessitate a new or updated fall risk assessment.
Such events may introduce new risk factors or escalate existing ones.
It leads to updated care plans that reflect the patient’s new needs and conditions.
Periodically During a Patient’s Stay in Healthcare Settings
Even in the absence of a significant health event, periodic reassess for a patient’s risk of falling during his stay in a healthcare setting is important.
This is because a patient’s risk factors can evolve over time due to factors like changes in medication, physical strength, balance, or mental status.
Regular reassessments help ensure that preventative measures remain effective and responsive to the patient’s current situation.
During Routine Health Check-ups
For older adults, routine health check-ups provide an important opportunity to assess fall risk. Regularly scheduled assessments in outpatient settings, such as during annual physicals, can help healthcare professionals identify and address risks early, potentially preventing falls before they happen.
Factors Considered in a Fall Risk Assessment
When the fall risk assessment is done, it is about to give a fall risk score for the patient ( or the senior ). One of the most important factors considered is the age which can be a significant factor in fall risk as the physical strength, balance, vision, and reaction time declines for the more aged people.
Additionally, older adults are more likely to have chronic health conditions that may contribute to falls.
Which is mandatory in the test is the historical falls of the patient, in fact, previous falls are one of the strongest predictors of future falls. This is why healthcare providers always ask about a patient’s fall history during an assessment.
The current physical conditions are checked during the test, for example, problems with mobility such as difficulty walking or moving from a sitting to standing position can contribute to falls. Cognitive impairments, such as those seen in conditions like Alzheimer’s disease or dementia, can also increase fall risk as they may affect a person’s ability to move safely. Other physical conditions like incontinence can increase fall risk as well, as the urgent need to use the bathroom can lead to hurried movements and falls.
Some mental health conditions may affect a person’s attention, concentration, or physical coordination so it has to be considered in the assessment.
Finally, medication is included in the assessmnet text because many medications, including those for blood pressure, sleep disorders, and depression, can increase the risk of falls due to side effects such as dizziness, low blood pressure, or impaired balance.
When the assessment is conducted at the senior’s home, environmental hazards are a key factor to consider. This includes poor lighting, cluttered walkways, loose rugs, lack of handrails in bathrooms, or any other environmental factors that could potentially lead to a fall.
How a fall risk assessment is done?
The process of a fall risk assessment can vary depending on the healthcare provider’s chosen method. The approach developed by the CDC (CDC) called STEADI is recommanded. It includes three critical components: screening, assessing, and intervention.
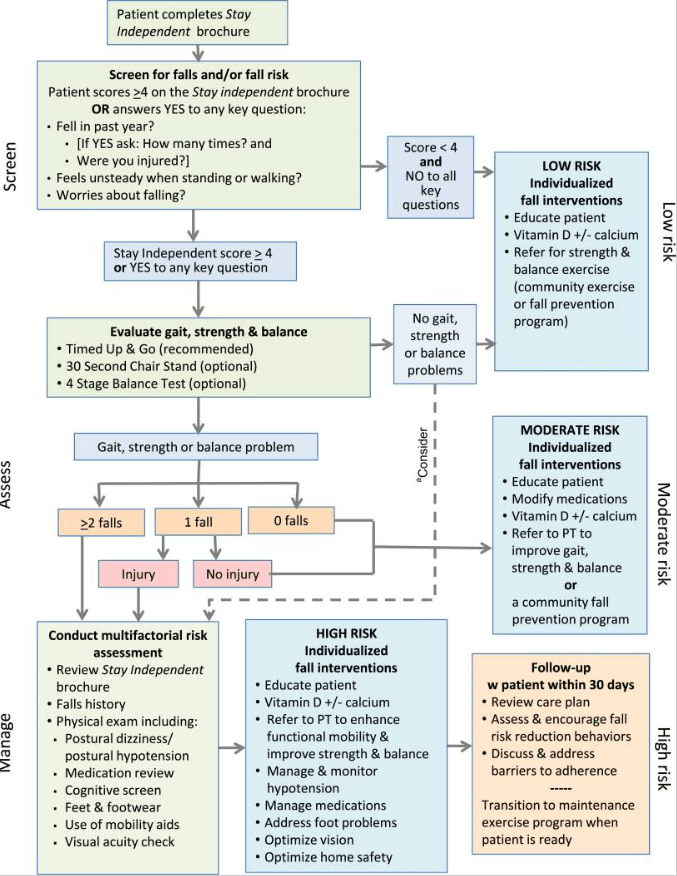
The Screening stage is based on three questions to gauge the risk of falling. These questions are:
- Have you fallen in the past year?
- Do you feel unsteady when standing or walking?
- Are you worried about falling?
The responses to these questions give healthcare providers initial insight into the potential risk of falling.
The assessing part of the process involves physical tests to assess the strength, the balance, and the gait. It will contain balance test, medications identification, potential home falling hazards…
At the end, the intervention: After the assessment, healthcare providers will recommend interventions based on the unique needs to help reduce your risk of falling.if for exemple, visual impairment were observed, the patient will be referred to ophthalmologist.
There are many other fall assessment tools available, and your healthcare provider might use different assessments based on the circumstances.
Types of Fall Risk Assessment Tools
To conduct fall risk assessments, healthcare providers use a variety of tools designed to systematically measure different aspects of a patient’s health and environment that could contribute to falls. Here are a few commonly used tools:
1. Morse Fall Scale (MFS): This tool measures fall risk based on factors such as a patient’s history of falling, secondary diagnoses, ambulatory aids, intravenous therapy, type of gait, and mental status.
2. Timed Up-and-Go (TUG): This tool assesses a patient’s mobility. It involves timing how long it takes a patient to stand from a seated position, walk three meters, turn around, walk back to the chair, and sit down.
3. Berg Balance Scale (BBS): This scale measures balance through 14 simple balance related tasks ranging from standing up from a sitting position to standing on one foot. The difficulty of the tasks gradually increases to test a patient’s balance capabilities.
4. 30-Second Chair Stand Test: This test is designed to assess lower body strength and balance. Patients are timed while they stand from a seated position and sit down again as many times as possible within a 30-second period.
5. 4-Stage Balance Test: This test assesses static balance by asking patients to hold four different standing positions for 10 seconds each, with the difficulty of the positions increasing each time.
6. Hendrich II Fall Risk Model: This model assesses fall risk in adults, taking into account factors such as confusion, symptomatic depression, altered elimination, dizziness, gender, any administered antiepileptics or benzodiazepines, and a patient’s performance in the “Get-Up-And-Go” test, a variant of the TUG test.
Intervention and Prevention Strategies
Once a fall risk assessment is done, healthcare providers can implement interventions tailored to the patient’s specific needs and identified risk factors.
These interventions aim to mitigate the risk of falls and ensure the safety and well-being of the individual. The strategies can be multidimensional, and often require the coordination of various professionals and involve the senior and his family.
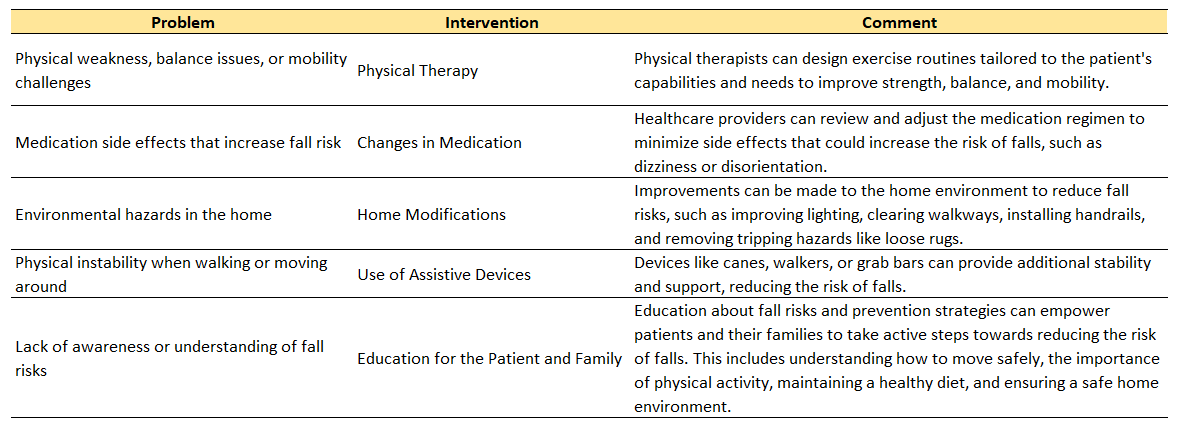
Physical Therapy and Medication Changes: Physical therapy can play a significant role in reducing the risk of falls by improving strength, balance, and overall mobility. Therapists may design exercises and routines tailored to the patient’s physical capabilities and fall risk factors. In addition, healthcare providers may review and adjust a patient’s medication regimen. Some medications can increase the risk of falls due to side effects like dizziness, sedation, or disorientation. A thorough medication review can help identify these risks and lead to necessary adjustments.
Home Modifications and Use of Assistive Devices: Environmental changes, especially at home, can significantly reduce the risk of falls. Home modifications can include improving lighting, clearing walkways, installing handrails, and removing loose rugs or other potential tripping hazards. Additionally, assistive devices like canes, walkers, or grab bars can be beneficial in providing extra stability and support.
Education: Lastly, education is a crucial part of fall prevention. This involves teaching the patient and their family about the risks and prevention strategies. Understanding why falls happen and how to prevent them can empower patients to take active steps in managing their own safety. This may include learning about safe ways to move around, the importance of regular physical activity, proper nutrition, and maintaining a safe living environment.
Important Resources about Fall Risk assessment:
- MedlinePlus Fall Risk Assessment
- Assessment and Management of Fall Risk in Primary Care Settings
- Lessons Learned From Implementing CDC’s STEADI Falls Prevention Algorithm in Primary Care
- How likely are older people to take up different falls prevention activities?
- Measuring balance in the elderly: validation of an instrument
- Falls risk assessment: a multifactorial approach

A seasoned SEO specialist and a writer for gaming, senior well-being, and ride-on toys. With an analytical mind, sharpened by 14 years of experience as a finance controller. His unique ability to create engaging content is only exceeded by his skill in leveraging SEO strategies, a talent driven by his love for numbers and patterns.









